Poster abstracts
Posters
This year there are traditional hanging posters only.
Registered delegates who attend the meeting may put up their poster. Deadline for poster registration is 15th August 2023.
The posters will be located in two areas: Max Rayne Foyer and the Atrium Well. Please refer to the doll’s house for location.
Please scroll down for abstracts. Click on the + after the title to open up more detail and the abstract text. Authors have been given a time slot to be available at their poster to answer questions (the time is noted after the title). Please note this is not mandatory.

Poster display and asking authors about their work
Only registered delegates may put up their poster at the assigned poster station.
The posters are located in two areas: Max Rayner Foyer and Atrium Well.
The posters are in cross formation with 8 posters in each (plus single poster board)
-
- Max Rayne Foyer poster boards 1 – 8
- Max Rayne Foyer poster boards 9 -16
- Max Rayne Foyer posters 17-18
- Atrium Well poster boards 1 – 8
- Atrium Well poster boards 9 -16
Each poster presenter has been assigned a 15 minutes slot to be at their poster during the conference to answer questions about their work.
Please refer to the time slot (either during Wednesday, Thursday or Friday lunch or Wednesday or Thursday afternoon tea break). The time slot is noted after the title. Please note this is not mandatory so authors may not be present during their alloted time. Thank you for your understanding.
Posters in the Atrium Well
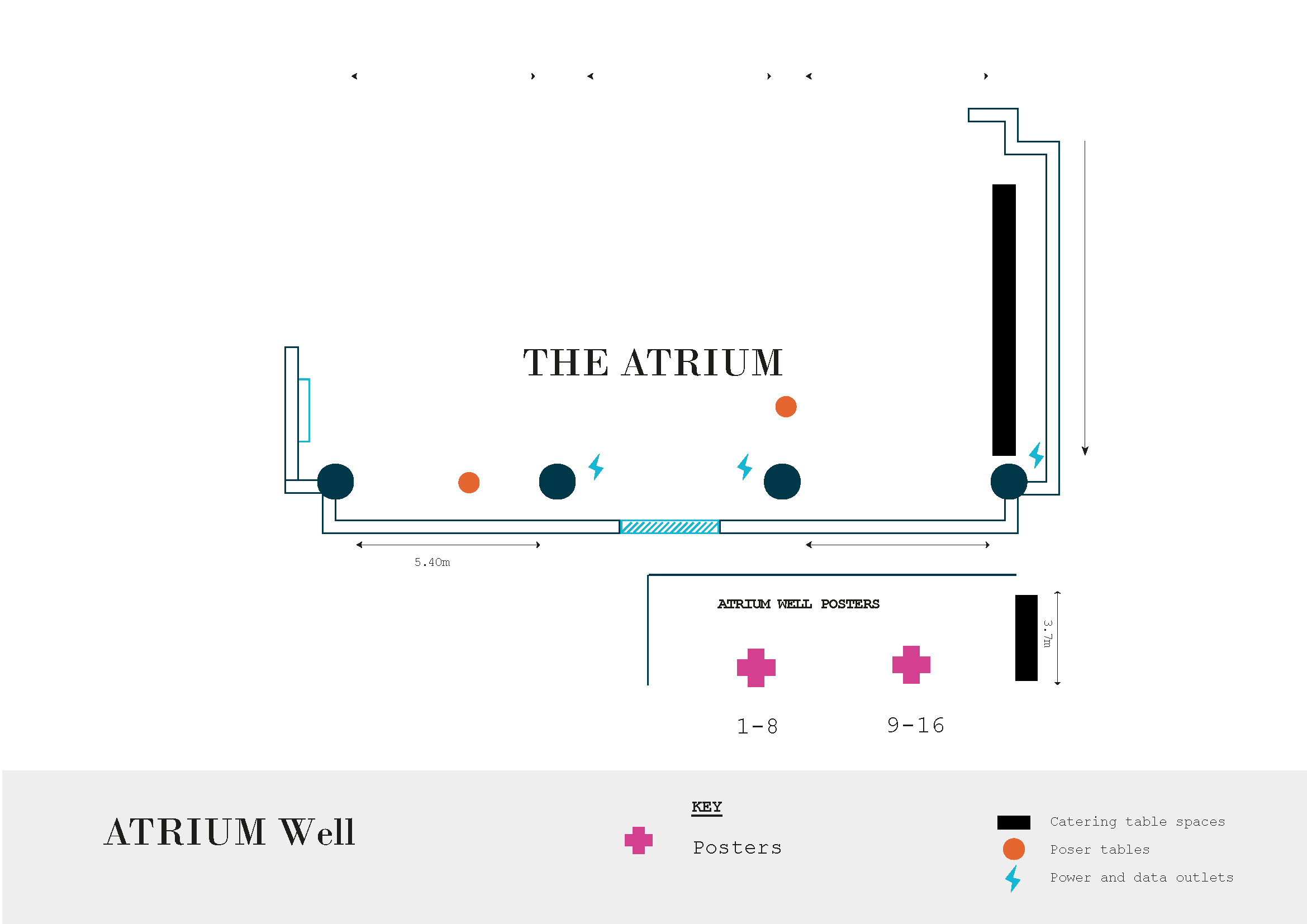
Atrium Well posters 1 -8
ABSTRACTS
Click on the + sign to open up abstracts
Secondary Idiopathic Intracranial Hypertension associated with Severe Aplastic Anaemia and Paroxysmal Nocturnal Haemoglobinuria - Wed 13.15 - 13.30
Dr T.Mannampat Shobh (CF), Ms S.Amarakoon (C), Bristol Eye Hospital
A 14 year old girl with severe aplastic anaemia and paroxysmal nocturnal haemoglobinuria requiring blood and platelet transfusion, presented with c/o severe headache and mild blurring of vision. She was on Ravilizumab, voriconazole , erythromycin , progesterone and was awaiting bone marrow transplantation.
Examination revealed bilateral haemorrhagic papilloedema and serous macular detachment . OCT disc confirmed the severe disc edema and OCT macula showed serous macular detachment .CT head and MR venogram confirmed papilloedema and excluded intracranial bleed, haemorrhage, hydrocephalus and cerebral venous sinus thrombosis. It showed features suggestive of raised intracranial pressure with dilated optic nerve sheaths and stenosis of lateral half of the right transverse sinus. Lumbar puncture was performed which showed opening pressure of 31cmH2O.
She was treated with Acetazolamide and therapeutic lumbar puncture (LP) was done. She went on to have five further therapeutic LPs to control intracranial hypertension.
She was symptomatically better in 10 days. Papilloedema resolved and OCT showed a marked reduction in the RNFL thickness and serous macular detachment. Bone marrow transplantation (BMT) was performed from a fully matched sibling. She has remained asymptomatic post BMT.
Previous case reports have documented the association between anaemia and raised intracranial pressure. This case shows importance of prompt treatment and resolution of Intracranial Hypertension with treatment of aplastic anaemia.
Post-operative evaluation of orbital fracture patients with diplopia in down gaze - Wed 13.30 - 13.45
S Poonoli (O), N Raoof (C) – The Royal London Hospital
Royal London Hospital is a major trauma centre for South east London. Due to this, high volumes of orbital fracture cases are seen by the ophthalmology. Management of orbital fractures when patients are asymptomatic in primary position, but symptomatic with diplopia in down gaze is challenging. Surgeries in these cases have risk of post-operative diplopia in primary position. However, we often explore this option when the patient is troubled by diplopia in down gaze.
Aims: This study aims to review the effects of surgery on patients who are symptomatic only at down gaze.
Method: We evaluated pre-operative and post-operative orthoptic findings of 7 patients aged between 24-79. These patients presented with diplopia in down gaze only, between January 2022- December 2022.
Conclusion: 2/7 patients were asymptomatic in all positions post-surgery. 5/7 patients continued to have diplopia in down gaze. This study highlights the importance of managing patient expectations in these cases.
Functional neurology: 3 unusual ophthalmic presentations - Wed 16.25 - 16.35
J Hoole (O), Leeds Teaching Hospitals NHS Trust
Functional neurology is a complex poorly understood disorder where there is physical response and no pathology is identified e.g. non epileptic seizures. It is therefore termed a problem with the functioning of the nervous system not due to damage or structural disease of the nervous system. There is often a combination of symptoms. Underlying triggers may be emotional and psychological help may be needed particularly in the more severe cases. Patients are often resistant to this. There is still a tendency for some orthoptists and other clinicians to believe symptoms are deliberately made up or put on as in true malingering. Common presentations to ophthalmology include functional vision loss, spiralling visual fields and near reflex spasm.
Three unusual cases are presented:
1) Increasing inability to walk in a teenager whilst waiting for decision to treat diplopia associated with decompensating deviation due to superior oblique weakness
2) A 70 year old with near reflex spasm after withdrawal of long term painkillers and sleeping tablets both of which may have been given for a functional problem in the first place
3) Opsoclonus myoclonus signs / symptoms
Orthoptists / other clinicians need to be alert to functional neurology and consider it as a differential diagnosis with true malingering in atypical as well as common presentations understanding that symptoms are real with an underlying emotional or psychomatic aetiology. Treatment in ophthalmology is unlikely to help particularly in the more extreme cases. Treatment and help will depend on local neuro and psychology services.
Half and half syndrome: A rare cause of diplopia - Thu 13.20 - 13.35
P H Downes (O), F Kirtley (C), Shrewsbury and Telford Hospital NHS Trust
An 81 year old man presented to A&E with symptoms of numbness and tingling on the right side of his face, pins and needles extending down into the right hand and sudden loss of the use of his legs. He was admitted to the stroke ward where MRI imaging identified a left pontine infarct. The stroke rehabilitation team referred him to orthoptics querying a possible diagnosis of 3rd nerve palsy causing diplopia, but this assessment led to a diagnosis of a left internuclear ophthalmoplegia and a left 6th nerve palsy.
Orthoptic assessment, 2 months after the onset of the stroke, demonstrated vision of 6/6 bilaterally, a lateral rectus restriction, as well as adduction deficit of his left eye and on the right, abducting nystagmus but no movement deficit. Although convergence was normal, there was left hypotropia caused by slight under action of the left superior rectus. Skew deviation was investigated and excluded. There was no evidence of facial palsy.
His co-morbidities included hypertension, chronic kidney disease, hypercholesterolaemia.
This patient is an example of half and half syndrome, an unusual presentation of diplopia and reported rarely. It is caused by a lesion involving the ipsilateral MLF, contributing half of the contralateral horizontal gaze palsy, and ipsilateral abducens nerve fasciculus, contributing half of the ipsilateral horizontal gaze palsy, whilst sparing the abducens nerve nucleus.
We present this case report to further expand the small evidence base of half and half syndrome and to help establish a wider knowledge of this rare INO plus condition.
MOG IgG optic neuritis in the paediatric population – an Irish case series - Thu 15.40 - 15.55
D Harford (T), D Townley, Galway University Hospital, Ireland
MOG IgG is a unique demyelinating cause with distinct features pertaining to treatment and prognosis. This is of importance as treatments are not universal for each cause of demyelinating disease. We describe two recent cases of MOG IgG associated optic neuritis in paediatric patients.
Case 1
A 10 year old female presented to eye casualty with a drop in vision in her right eye to CF from 6/5 accompanied by a swollen disc. MRI demonstrated a longitudinally extensive optic neuritis from globe to chiasm. Serum MOG IgG were found to be positive.
Case 2
A 6 year old female presented with a profound drop in visual acuity to 6/60 in her right eye accompanied by a swollen optic nerve head. Her MRI brain confirmed a long segment of T2 hyperintensity and swelling along the right optic nerve involving the intraorbital, intracanalicular and intracranial segments. Her blood work demonstrated anti-MOG antibodies.
Conclusion:
Our series highlights a number of clinical findings which help identify MOG IgG optic neuritis in children. Firstly, the profound visual loss which often accompanies a presentation of MOG IgG optic neuritis in children was evident. Secondly, MOG IgG associated optic neuritis is reported to be associated with longitudinally extensive lesions along the optic nerve which we also describe. Thirdly, optic nerve oedema is frequently present which we also describe. MOG IgG associated optic neuritis is associated with an excellent response to steroids. Therefore a high clinical suspicion and a timely diagnosis are important.
Lessons Learned from COVID-19 (discharge delays in Paediatric Orthoptic clinic) - Fri 13.15 - 13.30
S Kaneshanesan (O), Barts Health NHS Trust
Paediatric Ophthalmology is experiencing increasing demand, especially with the growing East London population. A retrospective audit on discharge trends on all Paediatric patients on Orthoptic ASI (n=1340) due to the closing of outpatients in response to COVID-19.
Outpatients closed from March 2020 to July 2020 and January 2021 to March 2021 in response to COVID-19, and all patient appointments were cancelled and added to ASI (Allocated Slot Issues). In line with Public Health England guidelines, all patient notes were reviewed and triaged using the traffic light system (Moorfields). Electronic patient records (appointments (CRS) + clinical (Medisoft)) were used to identify discharged patients and type of interaction i.e. SMART triage, telephone consultation, number of face-to-face or WNB.
(Preliminary 725/1340) SMART n=114, TC n=>70, F2F n=>304 WNB n=>38. Preliminary data indicates at least 39% of Paediatric Orthoptic patients were discharged from March 2020 to April 2023.
Clinical and parental caution influenced some delays in discharge, which led to a retention of patients who were safe to discharge and transfer eye care to local Opticians. COVID-19 gave an opportunity to change attitudes towards follow-up duration and need, and increased efficacy and efficiency of the Paediatric Orthoptic clinics.
Reviewing notes identified numerous patients who were safe to discharge, and led to increase efficacy for high demand service.
Clinical Characteristics of Isolated Inferior Rectus Palsy - Fri 13.30 - 13.45
LM Roberts (O), A Agrawal (SAS), VSY Geh (C) – Southend University Hospital, Mid and South Essex NHS Foundation Trust, Southend-on-Sea, Essex
Isolated inferior rectus palsy is a well-recognized but uncommon clinical entity and is conventionally stated to be associated with Myasthenia Gravis. There is limited literature available on this condition. The aim of this report was to elucidate the aetiology and clinical characteristics of isolated inferior rectus palsy.
We undertook a 3-year retrospective study of patients with a diagnosis of isolated inferior rectus palsy. Records of 12 patients were available to be reviewed who attended between January 2021 and February 2023.
The mean age at diagnosis was 63.5 years (range 35 to 83 years). There were 5 men and 7 women. The main clinical presentations consisted of hypertropia of the affected eye, motility limitation in abduction and depression. Ten were tested for Myasthenia Gravis of which diagnosis was confirmed in 3 patients. Out of the remaining cases, the aetiology was unknown in one, four were microvascular and 2 had other causes like trauma and blood dyscrasia. Ptosis was found in 1 of the cases of Myasthenia Gravis.
The main aetiologies of isolated inferior rectus palsy involved myasthenia and microvascular events. Patients who present with isolated inferior rectus palsy should be investigated for Myasthenia gravis.
A novel phenotype associated with the GJA8 c.280G A p.Gly (94Arg) variant - Fri 13.45 - 14.00
J Gilmour-White (T), A Churchill (C), M Tooley, Bristol Royal Infirmary
GJA8 is a gene that encodes for connexin 50, a transmembrane protein that plays a crucial role in lens development and homeostasis. A wide range of mutations in GJA8 have been identified as the underlying cause for a spectrum of ocular phenotypes. Notably, the GJA8 c.280G>A p.Gly(94Arg) variant has been established as a likely pathogenic mutation. Previous studies have documented three cases in the literature that demonstrate a phenotypic spectrum consisting of aphakia, corneal opacity, microphthalmia, coloboma and glaucoma. In this report, we present a novel case of this variant with bilateral congenital aphakia, bilateral aniridia (iris tissue remnant visible in the periphery with transillumination), and corneal opacity. While coloboma of the iris and optic nerve have been reported in the past, we believe this to be the first documented case of aniridia associated with the GJA8 c.280G>A p.Gly(94Arg) variant. PAX-6 variants, which are a well-recognised cause of aniridia, were excluded. This case expands the current understanding of GJA8 variants and their associated phenotypes and underscores the importance of genetic GJA8 screening in individuals with developmental eye abnormalities.
Atrium Well posters 9 -16
ABSTRACTS
Click on the + sign to open up abstracts
Use of anti-Vascular Endothelial Growth Factor (antiVEGF) in the Treatment of Retinopathy of Prematurity (ROP), A Systematic Review and Meta-Analysis - Wed 13.15 - 13.30
S.J Udakumbura (SL), P Watts (C), University Hospital of Wales
Retinopathy of prematurity (ROP) is one of the leading causes of blindness in children worldwide. The management of ROP has been revolutionised with the introduction of intravitreal anti-vascular endothelial growth factor(antiVEGF) agents. This review evaluates the safety and efficacy of intravitreal antiVEGF agents when used either as monotherapy, or in combination with laser/cryo in type 1 ROP.
A comprehensive literature search was conducted from 2000 to April 2022 using the following databases PubMed, EMBASE and CINHAL. Total of 12 randomised controlled studies (RCTs) and 7 comparative studies were selected after critical appraisal. RCTs were included in the meta-analysis.
There were 4628 eyes of 2571 infants with type 1 ROP were identified from the included studies. A meta analysis showed no statistically significant difference in retinal detachment, ROP recurrence, mortality and cerebral palsy between standard treatment (laser/cryo) and antiVEGF mono therapy. AntiVEGF mono therapy may reduce the risk of refractive errors in childhood compared to standard therapy. No significant risk of acute and long-term systemic complications noted with antiVEGF therapy.
AntiVEGF agents, as mono therapy is non inferior to standard therapy after evaluating for risk of retinal detachment and recurrence of ROP in infants with type 1 ROP. The data is not sufficient to make strong conclusions favouring routine use anti-VEGF agents as monotherapy in all types of type 1 ROP. Hence, further large scale RCTs with longer fallow up period are necessary to evaluate the safety and efficacy of antiVEGF agents for type 1 ROP.
References: 1. Mintz-Hittner HA, Kennedy KA, Chuang AZ. Efficacy of Intravitreal Bevacizumab for Stage 3+ Retinopathy of Prematurity. N Engl J Med. 2011 Feb 17;364(7):603-15
2. Stahl A, Lepore D, Fielder A, Fleck B, Reynolds JD, Chiang MF, et al. Ranibizumab versus laser therapy for the treatment of very low birthweight infants with retinopathy of prematurity (RAINBOW): an open-label randomised controlled trial. The Lancet. 2019 Oct 26;394(10208):1551-9
The Prevalence of Peripapillary Hyperreflective Ovoid Mass-like Structures (PHOMS) in Suspected Papilloedema in Children - wed 13.30 - 13.45
S Rehan (T), L Pratt (T), J West (T), P Watts (C), University Hospital of Wales, Cardiff
Suspected papilloedema is a frequent cause of referral to paediatric ophthalmology clinics. To allow prompt assessment and manage demand, we run a virtual suspected disc swelling clinic. In these clinics, OCT disc images are taken and reviewed separately by an ophthalmologist. Recent publications have described a new finding called peripapillary hyperreflective ovoid mass-like structures (PHOMS) that may simulate papilloedema. We aimed to retrospectively review the OCTs from these virtual clinics for the presence of PHOMs and report their frequency.
124 patients between 31st August 2016 and 17th March 2021 were appointed to the virtual clinic. 13 patients did not attend, and 1 had ungradeable images. In total 110 patient scans were reviewed by 3 assessors. The OCT appearance was compared with previously published images and descriptions of PHOMS. The agreement between assessors was also recorded.
The average age was 11.2 years (SD 3.4 years). PHOMS were identified in 74 patients (67.3%). 56.8% were bilateral. PHOMS were most commonly seen in association with other identified causes of pseudopapilloedema e.g. tilted disc and drusen (81.3%), but were also common in true disc swelling (66.7%) and otherwise healthy discs (55.4%). There was a high rate of agreement between assessors (Fleiss’ kappa 0.97)
Misdiagnosis of true disc swelling can lead to unnecessary and invasive tests. PHOMS are found frequently within the paediatric population referred for suspected disc swelling. They may be an independent cause of pseudopapilloedema but are often seen in conjunction with other diagnoses e.g. true disc swelling or drusen.
Tales of the Unexpected! The Story of the Princess and the Satsuma—A rare presentation of Abducens Palsy - Thu 13.20 - 13.35
N V Corbin (O), B Cuckson (Op), M Shamir (SAS), North Cumbria Integrated Care NHS Foundation Trust, Carlisle
15 month old female, born at full term, presented to the orthoptist with a 6 day history of isolated vomiting, lethargy and 4 days of sudden onset left esotropia. Three consultations by GP had been undertaken without concerns raised.
Orthoptic examination found vision of 0.5 logMAR with Cardiff Cards. Approximately 20 prism dioptre esotropia for near and distance on cover test, with a marked restriction of abduction of the left eye. Dilated examination showed bilateral hypermetropia within normal limits for age. Fundoscopy showed left papilloedema with the fellow eye appearing normal. General observation showed ataxic gait, lethargy, prominent forehead, and reduced use of right arm.
Immediate admission to paediatrics with MRI under sedation. Radiological findings showed a mass in the lateral ventricles measuring 5.6cm x 6.1cm (equivalent to a satsuma) resulting in complete hydrocephalus, and a retro-cerebellar arachnoid cyst. Immediate management on dexamethasone and rapid deterioration resulting in specialist intubated transfer to tertiary centre in Newcastle. Immediate surgery for Extraventricular Drain (EVD), followed by surgical excision of mass by temporo-occipital craniotomy.
Spontaneous resolution of left abducens palsy following surgery. Histo-pathology showed Choroid Plexus Papilloma (CPP), WHO Grade 1. Normal developmental milestones resumed.
CPP is a very rare presenting aetiology of acquired Abducens Palsy, accounting for 0.4% of CNS tumours. Its slow growing nature often results in 6 months or more of symptoms before diagnosis. In a child with unexplained vomiting/nausea and headache and neurological signs, immediate imaging investigations should be sought.
Acquired Monocular Nystagmus in Pilomyxoid Astrocytoma - Thu 15.40 - 15.55
TKJ Chan (C), QX Lim (T), N Hall (T), A Stan (C), K Orr (C), Princess Alexandra Eye Pavilion, Edinburgh
Acute onset monocular or asymmetric nystagmus is rare in the paediatric population. This tends to be seen in children in three scenarios: monocular visual loss; spasmus nutans; or as a presenting feature of an chiasmal/midbrain lesion. We aim to report a rare case of acute monocular nystagmus in a 4-month-old girl whose radiological and histopathological findings confirmed a diagnosis of pilomyxoid astrocytoma.
A 4-month old girl presented with right monocular nystagmus associated with poor feeding and weight loss. She was born full term via spontaneous vaginal delivery, weighing 7lbs 11oz following uncomplicated pregnancy. Examination showed monocular pendular nystagmus with horizontal and rotary component in the right eye only. There was no head bobbing or torticollis. Pupillary reflexes were normal with no relative afferent pupillary defect. She had symmetrical corneal reflexes and full eye movements. Dilated fundus examination showed healthy discs and normal fundi. Cycloplegic refraction showed +3.00D/+2.25D at 110° in right eye and +0.50D/+1.50D at 80° in left eye.
Subsequent investigations showed radiological findings of a highly aggressive brain tumour in the suprasellar region with widespread metastases in the posterior fossa, Circle of Willis, intracranial optic nerves and in C2, C6 and C7 spinal canal. Histo-immunopathology confirmed features of pilomyxoid astrocytoma. She underwent debulking surgery, ventriculoperitoneal shunt insertion and chemotherapy. Despite this, the disease progressed and she sadly passed away 5 months after initial presentation.
This case highlighted the importance and low threshold for neuroimaging in children presenting with acquired monocular nystagmus especially in those younger than 2 years old.
Novel inferior oblique muscle Y splitting procedure to minimize the anti-elevation syndrome - Fri 13.15 - 13.30
Amar Pujari (C), New Dehli, India
To describe novel Y splitting procedure of inferior oblique muscle to mitigate the anti-elevation syndrome.
A pilot, prospective interventional study was undertaken to assess the effect of inferior oblique muscle Y-splitting in patients with unilateral 3+ or more overaction. To correct primary gaze hypertropia and the excyclotorsion, a Y-splitting procedure was performed (along with routine horizontal muscle surgery as per the deviation) in 14 subjects. The effect of surgery was assessed at baseline and at 6 months post-intervention.
The mean age of 14 subjects was 25.14 +/- 7.70 years. The mean pre-operative hypertropia, excyclotorsion and inferior oblique muscle over-action was 18.42+/- 3.50 PD, 14.14+/- 2.65 degrees, and +3.21+/- 0.42 respectively. Following surgery this was reduced to 1.57+/- 1.74 PD of residual hypertropia (a net correction of 16.85+/- 2.31 PD, p=0.005), 3.85+/- 1.46 degrees of residual excyclotorsion (a net correction of 10.28+/- 1.72 degrees, p<0.05), and +0.28+/- 0.46 of residual inferior oblique over-action (a net correction ~+3) at the end of 6 months. Amongst fourteen patients, three patients still experienced residual/variable anti-elevation effect, and during the study period none of them experienced any adverse event and none of them required any additional surgeries.
While anteriorizing the inferior oblique muscle to correct primary gaze hypertropia and the excyclotorsion, a novel “Y splitting” procedure can be followed to achieve the desired results with mitigated anti-elevation effect.
Impact of red light from light-emitting diodes on subfoveal choroidal thickness and colour contrast sensitivity: proof-of-concept study - Fri 13.30 - 13.45
J Lam (CF/C), A Dahlmann-Noor (C), G Jeffery (P), Moorfields Eye Hospital NHS Trust
Daily viewing of low-level red laser light can slow progression of myopia in children, but effects on foveal photoreceptor health are unknown. An increase in subfoveal choroidal thickness (sfChtT) may play a role in the mechanism of action of red light in modulating scleral remodelling and axial elongation. We conducted this proof-of-concept study to study the short-term effects of viewing 670nm light from red LEDs on sfChT.
Six adult healthy volunteers viewed 670nm light from red LEDs for 3 minutes; three repeated the application once more later in the day. We measured sfChT on enhanced-depth imaging optical coherence tomography scans before and over 24 hours after the first viewing session.
Median sfChT increased from 257.5um (interquartile range IQR 165.8 to 331.6) at baseline to 280um (IQR 177 to 368.6) at 30 minutes, where it remained until 24 hours (n=6, p<0.05). Mean difference in sfChT from baseline to 30 minutes was 21.5(SD13.0)um, and to 24 hours, 18.1(SD23.6)um. Mean difference in sfChT from baseline to 24 hours in those participants who used the red-light treatment once (n=3) was 1.3 (SD1.8)um, and 34.9(SD23.3)um in those who had a second application later in the day, indicating that the second application may have prolonged the effect on sfChT increase (p=0.03).
Viewing red light from LEDs increases sfChT, an early biomarker of a therapeutic effect on scleral remodelling and axial elongation in progressive myopia in children, similar to that reported for low-level laser light. Red light from LEDs enhances photoreceptor function by increasing mitochondrial respiration, and possibly by improving oxygenation of retina and sclera downstream of an increase in choroidal perfusion.
Spectrum of visual dysfunction detected by a novel testing protocol within the Special School Eye Care Service - Fri 13.45 - 14.00
RF Pilling (C), M Musleh (T), A Mankowska (Op), C Viner (Op), A Green (Op), University of Bradford
NHS England Special School Eye Care Service (SSECS) offers in-school visual assessments to children with special needs. The recommended testing strategy includes visual acuity, contrast sensitivity (CS), visual field (VF), stereoacuity, accommodation, eye movements (EM), refraction and parent-completed questionnaire (CVI5).
The aim of this evaluation is to report on the outcomes from the first cohort assessed by the locally commissioned service.
The service operates with opt-out consent. Data are routinely submitted to NHSEngland. The order of testing and tools used were determined by the optometrist to maximise each child’s engagement. All children on whom testing was attempted were included.
78 case records were identified. The mean age of children tested was 9.6 years (range 7-12y). All six visual function tests were completed by 44% patients, with a mean of 5. (range 2-6). Visual acuity was <6/15 in 31% cases.The most frequently omitted test was stereopsis (60% children completed), with >90% patients completing VF, CS, EM and accommodation. Only 20% children had a normal response to all tests. 44% parents returned the questionnaire; parents were more likely to complete this if their child had low visual acuity.
We found a higher proportion of special needs children with atypical visual function compared with previous studies. Children can engage well with the majority of tests with the possible exception of stereoacuity. The SSECS may have a role in identifying children who warrant further assessment for CVI related visual dysfunction.
Posters in Max Rayne Foyer
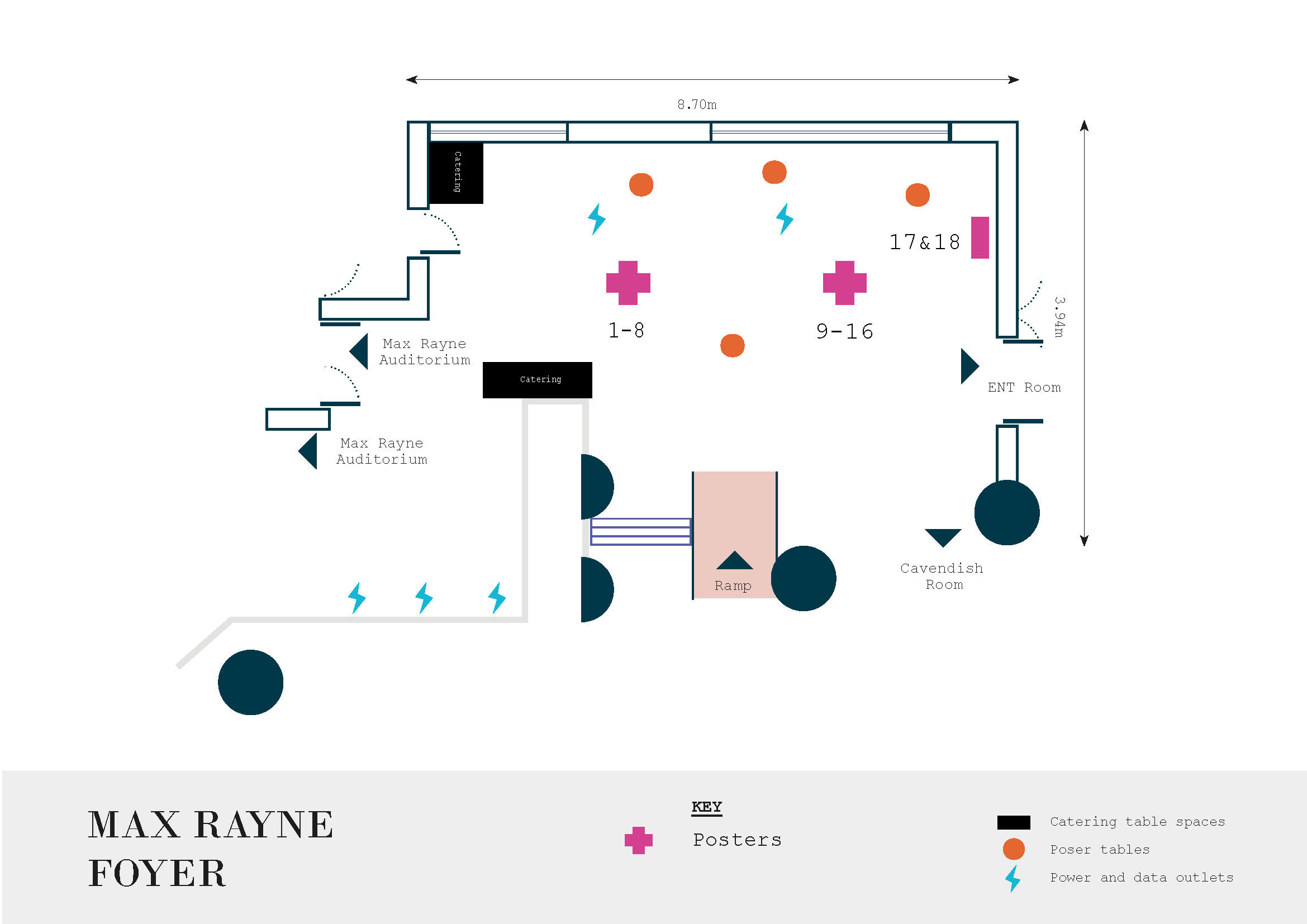
Max Rayne Foyer posters 1 -8
ABSTRACTS
Click on the + sign to open up abstracts
Usability of Delivery Aid for Vernal Keratoconjunctivitis Single-Dose Treatment - wed 13.15 - 13.30
K N Lebron (F), A Dahlmann-Noor (C), Moorfields Eye Hospital NHS Foundation Trust
Usability of eye drop containers is particularly important for patient compliance when treating chronic eye diseases like vernal keratoconjunctivitis (VKC), glaucoma and ocular surface disease. Factors affecting treatment adherence include the convenience of use of the medication. The findings suggest that preferences may differ including the mechanical characteristics of the packaging or what the drop control is like. Santen has developed Dropaid VKC Single-Use, a delivery aid for use in combination with Verkazia in single use containers, that aims to help caregivers instill eye drops.
Eligible participants used Dropaid VKC Single-dose to administer CATIONORM PRO emulsion drops to a medical dummy, and then evaluated the usability characteristics of the delivery device by completing a questionnaire. Thirty adult participants were recruited and the usability was assessed through drop control, which was performed by an observer.
Thirty patients completed the study. Most of the participants were females between 41 and 50 years old. 56% of the participants had experience using multi dose treatment and 43% using single dose drops, average of 3 to 5 years of overall experience. 76% of the participants found the general usability of the Dropaid VKC Single-dose container very easy, however 53% would recommend its use, 30% maybe and 17% would not recommend it. Most of the participants use the right hand to instil the drops, applying to the left eye first with approximately 2 drops per try.
Dropaid VKC Single-dose is a helpful tool to help caregivers instill eye drops from single use containers.
Do my discs look big? - wed 13.30 - 13.45
C McAtamney (O), P Anketell (O), A McCaw (o), S George (C), Belfast Health & Social Care Trust
Swollen discs can be a marker of a potentially sight or life threatening condition. In Belfast Health & Social Care Trust (BHSCT) an increase in referral rates has been noted (0.9/month pre-2016, 3.3/month in 2019, Stewart et al, 2017). The COVID pandemic reduced access to hospital eye services making assessment challenging therefore an orthoptic delivered swollen discs clinic was developed which includes orthoptic assessment, imaging and virtual review by a consultant.
The database for all children attending the clinic was interrogated for this study. Visual measures and clinical outcomes were recorded for analyses.
This study reports on 217 children completed the clinic process; new=137, review= 80. Of the new patient were referred from an optometrist n=118, eye casualty n=4, paediatrician n=6, paediatric ophthalmologist n=5. Following review of the clinic reports 57% of all patients were discharged, this rises to 66% of all new patient referrals.
The development of this service has increased capacity within the paediatric ophthalmology service. Post COVID this service has continued for children requiring investigation of potential swollen discs. Extended scope training has been developed for orthoptists to with appropriate training to commence image review.
TeleROP NI - A Service Improvement Initiative for Paediatric Ophthalmology in Northern Ireland - wed 16.25 - 16.35
J Kearney (N), E McLoone (C), L Hamilton (o), Belfast Health & Social Care Trust
Every year in Northern Ireland, approximately 300 preterm infants require Retinopathy of Prematurity (ROP) screening. While fewer than 5-7% of the infants screened eventually require treatment, all eligible preterm infants must be screened at 1-2 weekly intervals from 31 weeks gestational age onwards. ROP is a time-sensitive eye condition in infants, which if undetected can result in lifelong blindness. This has life-changing implications for the infant and their family and significant adverse medico-legal implications for health care professionals and the National Health Service.
In September 2021, due to a paucity of Paediatric Ophthalmologists in Northern Ireland (NI), a novel three-tiered approach was introduced to manage the regional ROP service (TeleROP-NI). This consists of a regional ROP Clinical Coordinator, a weekly virtual ROP Multidisciplinary Team meeting and retinal imaging. As part of this initiative, non-medical ROP Imagers have undergone rigorous competency based consultant-led training in retinal imaging using handheld wide-field cameras. This poster summarises the development of a TeleROP-NI service improvement initiative and highlights a different approach for managing ROP screening and treatment.
Management of acutely acquired esotropia with botulinum toxin - Thu 13.20 - 13.35
N Patel (O), S Jain (C), R Jolly (C), Royal Free Hospital, London
We looked at the investigation and management of a child who presented with a new onset incomitant esotropia. We specifically look at the use of botulinum toxin (BT) as a diagnostic tool but also the possibility for its use as a therapeutic measure.
A 2-year-old male presented with an acute onset right esotropia with a significant abduction limitation. The orthoptic assessment showed a minus 4 limitation of abduction and a significant right face turn. Patching of the left eye could not prove an improvement in motility and binocularity was maintained with the face turn but diminishing with each visit. This led to a diagnostic dilemma with sixth nerve palsy being considered as a possible diagnosis. Considering the clinical features and acute onset deviation we did an MRI which was normal and then subsequently a decision made to inject 10 units of dysport BT into the right medial rectus under GA. The needle was held in place for 90 seconds to avoid inducing ptosis or a vertical deviation.
The BT injection showed an excellent outcome as full abduction was proven in this child, with good binocularity in primary position and no residual deviation or compensatory head posture at three months following the procedure.
There is a limited consensus with regards to the best management of children presenting with acute onset esotropia especially those simulating a sixth nerve palsy.
The use of BT has showed an excellent outcome in this child and should be considered an option both as a diagnostic tool and a therapeutic measure in other children presenting with acute acquired incomitant esotropias.
Home visual acuity testing in young children using a smart phone App - Thu 15.40 - 15.55
Ahmed Ghoneim (CF), M Abbas (O), S Ludden (O), D ElFadaly (CF ), A Dahlmann-Noor (C) (P), Moorfields Eye Hospital, London
VA is a core component of any eye-health consultation and management decisions.
OKKO-Health have developed a VA-app for home acuity-testing in young children by parents/carers, using pictorial Auckland Optotypes (TAO).
We approached children under the age of 16 years attending our clinics.
We recorded logMAR acuity at 3metres distance with Kay pictures or letters (Thomson-chart). Parents/carers were given an iPhone-XS with pre-installed OKKO App. We recorded age, gender, and worse-eye visual acuity.
We collected data from 46 children, mean age 6.5 standard deviation 3.3 years; 23 boys. 21 had amblyopia/refractive error/strabismus, 13 a lid/ocular surface condition, 5 congenital glaucoma, 5 healthy eyes/normal-for-age vision, and 1 each pseudophakia or anterior uveitis.
Median OKKO-TAO acuity was 0.19 interquartile range 0.00 to 0.40 and median VA was 0.13 logMAR (IQR 0.03-0.21). Mean difference between OKKO and reference standard was 0.08 logMAR, SD 0.24, 95 % CI (-0.15 to -0.04). Intraclass correlation coefficient was 0.7, 95% of measurements between +/- 0.48 logMAR
Results showed agreement between reference standard and TAO-element of the OKKO prototype. Limitations that near acuity (OKKO-app) may over-estimate distance acuity. Comparing the vanishing-optotype, picture-only OKKO-TAO-prototype with a non-vanishing optotype reference standard affects our comparison, SD of 0.24 limits implementation into practice.
The updated version of the OKKO-Health app includes other targets, with a mechanism for brightness, grey scale and continuous measurement of distance between child and front-camera all to increase test performance. Evaluation is in progress.
Ocular Manifestations in Children with Autism Spectrum Disorder - Fri 13.15 - 13.30
U KARAMCHANDANI (FD), N Oluonye (C), M Moosajee (C), Moorfields Eye Hospital, London
Evidence suggests abnormal visual and sensory processing contributes to developmental delays in children with autism spectrum disorder (ASD). However, current studies on ocular manifestations in these patients are limited by samples sizes, partly due to behavioural challenges during assessments. We therefore aimed to evaluate this within the large Moorfields database.
Moorfields Eye Hospital records were searched for “ASD”, “Autism”, and “Autistic” to identify patients with this diagnosis. The ocular diagnoses and visual acuities were then recorded for patients aged under 20-years-old.
The study identified 1,245 patients with ASD, 870 demonstrated ocular manifestation(s). The mean visual acuity LogMAR (mVA) across the cohort was 0.40 (SEM: 0.17, range: -0.70-3.00). The most common conditions were strabismus (38%, mVA: 0.25, SEM 0.01, range: -0.70-1.50), then refractive errors (33%), amblyopia (7%), and retinal pathologies (6.9%, mVA: 1.12, SEM 0.10, range: -0.70-3.00). Sixty patients had confirmed genetic diagnoses with the majority being Lebers congenital amaurosis (23%, mVA: 2.58, SEM: 0.17, range: 0.80-3.00).
The prevalence of strabismus, refractive errors and amblyopia is much higher in this cohort than the UK paediatric population. Those with retinal pathologies, including dystrophies, retinopathy of prematurity, detachments, and genetic diagnoses, had low visual acuities or only perception of light. Given the importance of visual cues in childhood development, this may explain behavioural challenges.
Ocular manifestations occur more frequently in patients with ASD, and this may contribute to their behavioural and developmental delay. It is important to perform an ophthalmic evaluation and provide the necessary management if required.
Does ciclosporin A 1mg/ml cationic emulsion reduce the need for steroids in atopic, blepharo- and vernal keratoconjunctivitis? - Fri 13.30 - 13.45
A Dahlmann-Noor (C ), M Hingorani (C ), K Muthusamy (C ), C Roberts (C ), V Calder (P), NIHR Moorfields Biomedical Research Centre
Topical ciclosporin A 1mg/ml cationic emulsion (CsA) has recently received marketing authorisation in North America for vernal keratoconjunctivitis (VKC). It may reduce the need for topical corticosteroids and contribute to maintenance treatment of VKC, and also atopic and blepharokeratoconjunctivitis (AKC, BKC).
We reviewed the medical records of 485 children treated with CsA between 2015 and 2021, including 209 with VKC, 99 with AKC and 145 with BKC.
Median age at start of treatment was 9.7 years (IQR 7.2 to 12.8 years), 333 boys (62.5%). Data were available for 12 months before/after starting CsA in 227 cases. The median number of inflammatory episodes requiring topical corticosteroids fell from 3 (IQR 2-4) to 1 (IQR 0-2), excluding steroid prescriptions concomitant with the first CsA prescription; Wilcoxon signed ranks, 2 tailed, p<0.01. The number of clinic visits fell from a median of 4 (IQR 3 to 6) to 3 (IQR 2 to 5); Wilcoxon signed ranks, 2 tailed, p<0.01). Stinging was a common adverse effect (4.7%); skin rash was unusual (0.6%). The most common reasons for discontinuation was a perception that the medication was no longer needed (32.8%) or the family not requesting, or the general practitioner not issuing, a repeat prescription (18.8%).
Csa 1mg/ml cationic emulsion reduces the need for topical corticosteroids and hospital visits and may improve the quality of life of children and families. Information and communication need to improve to raise awareness of VKC, AKC and BKC as chronic conditions requiring long-term treatment.
Therapeutic botulinum toxin use in paediatric strabismus, the Sheffield experience - Fri 13.45 - 14.00
T Liu (T), M Naguib (FD), S Gosling (O), A Tandon (C), Sheffield Children’s NHS Foundation Trust
Surgery is regarded as the mainstay treatment of paediatric strabismus. Botulinum injections, such as Botox, have emerged as a viable alternative. The procedure involves less trauma to the eye and is more tolerable in comparison to more lengthy and intense surgical options, especially in the paediatric population. This study aims to explore the efficacy of Botox in the management of paediatric strabismus.
A retrospective single centre study was conducted at a tertiary hospital ophthalmology unit. 41 patients were identified via electronic patient records between 2016 to 2021. Data collected included; age at time of procedure, primary and secondary diagnosis, muscles injected, Botox units, if patients underwent combined squint surgery, pre-operative and post-operative angle measurements, complications and whether patients underwent repeat Botox or further surgery.
Of the 41 patients, 80.5% underwent Botox injection to both medial recti. The mean difference in angle size by the third visit was a reduction of 23D. 14.6% required repeat botox after the third visit and 24.4% underwent further squint surgery later on. Of the 53.7% who experienced complications, 72.7% consisted of ptosis that self-resolved.
Botox injections may be effective in treating strabismus but the effect may be temporary and patients may still require repeat injections or surgical treatment in the future. Overall, there may be a place for the use of Botox injections in the management of paediatric strabismus as an option prior to or after strabismus surgery for those who would like to opt for a less invasive procedure.
Max Rayne Foyer posters 9-16
ABSTRACTS
Click on the + sign to open up abstracts
Have SARS-CoV-2 virus (COVID-19) lockdown restrictions impacted the prevalence and severity of retinopathy of prematurity in a London population? - wed 13.15 - 13.30
K Reed (T), S Bazeer (T), I Hossain (T), D El Fadaly (CF), M Tsimpida (C), H Patel (C), A Das (C), A Khaier (C), M Posner (C), Queens Hospital, Romford
During the COVID-19 lockdowns in 2020 numerous global neonatal intensive care units (NICU) reported reduced incidence of pre-term births. Retinopathy of prematurity (ROP) is a vision-threatening disease that affects premature infants. We hypothesised that there may be a corresponding reduction in incidence and severity of ROP.
Comparison of birth weight (BW), gestational age (GA) and ROP stage from three East-London NICU during the UK lockdown period March to October 2020 matched with equivalent dates in 2019. Inclusion criteria; GA<32 weeks or BW<1501g.
264 ROP-screened pre-term babies included; 138 in 2019, 124 in 2020. 65 (46%) in 2019 and 46 (37%) in 2020 were diagnosed with maximal ROP grades 1-3. Babies were of similar GA (p=0.6) and BW (p=0.9) across the cohorts. There was, however, a statistically significant difference in the severity of ROP with 13 (9.4%) 2019 babies vs 5 (4%) 2020 babies diagnosed with stage 3 ROP requiring treatment (p<0.05).
Fewer pre-term babies were born in 2020 compared to the same time period in 2019. Of the pre-term babies that were born, fewer were diagnosed with ROP and fewer still had stage 3, treated ROP. The underlying reasons for this are uncertain and require further investigation but postulated suggestions include decreased incidence of maternal infections, decreased maternal activity and improved air quality.
This mirrors findings from a similar study in Japan indicating a reduction in sight-threatening ROP in babies born during Covid lockdown. Further investigation is required to determine a cause-effect relationship and to further inform expectant mothers.
HSV2 induced Acute Retinal Necrosis in an 8-year-old child - wed 13.30 - 13.45
C M Luxhoj (FD), R Jolly (C), H Petrushkin (C), D Hanumunthadu (C), Royal Free Hospital, London
An 8-year-old male presented acutely with a red, itchy and painful right eye (RE). He had a past medical history of mild asthma, allergic rhinitis and a RE convergent squint but no other ocular history or relevant family history.
Visual acuity was RE 6/36 unaided, left eye (LE) 6/9 unaided. There was significant RE conjunctival hyperaemia and anterior chamber inflammation (cells 3+, flare 3+) with inferior keratic precipitates. Fundus examination showed vitritis in the RE with blurred disc margin, periphlebitis, temporal haemorrhages and retinitis. The LE was normal. Systemic assessment, autoimmune screen, syphilis serology and toxoplasma serology were normal.
Urgent aqueous biopsy was performed (which confirmed HSV2) with concurrent intravitreal foscarnet treatment.
Systemic antivirals were commenced: intravenous acyclovir followed by valaciclovir 20 mg/kg and subsequent addition of oral prednisolone.
Inflammation improved initially with treatment but progressed to secondary retinal detachment at two weeks post presentation. Prior to retinal detachment, the patient described worsening vision (to perception of light) but with stable ocular findings (no retinal detachment and improving ocular inflammation). Electrophysiology at this time was consistent with vision of 6/36 RE possibly indicating functional overlay.
HSV2 associated acute retinal necrosis (ARN) is a rare condition, particularly in children, and may present with no previous significant ocular or medical history. Functional overlay has the potential to further complicate management, especially in such complex cases.
Development of a low-cost simulation model for neonatal speculum insertion - wed 16.25 - 16.35
H St Ledger (O), S Jain (C), R Jolly (C), Royal Free Hospital, London
Retinopathy of Prematurity (ROP) screening is a vital service for premature and low birth weight babies to identify early changes in the vasculature of the retina. One of the challenges we encountered while training orthoptists to participate in the service was the use of a neonatal speculum. We have devised a low-cost, high-fidelity model to help simulate this technique and up-skill clinicians.
A linear horizontal superficial incision was made in the skin of the grape using a no 15 blade to replicate the palpebral fissure. The opening created, allowed a neonatal speculum to be repeatedly placed and removed whilst observing for any underlying trauma to the grape.
The model was used by trainees, orthoptists, and non-medical individuals, and their pre and post procedure confidence was evaluated. We derived validity of the simulation by speaking to consultants and assessing their opinions with regards to how reliable the model was.
We observed an increased confidence in using the neonatal speculum following practice on the model eye.
This simple, readily available, and cost-effective simulation model was demonstrated to have a real-life clinical application, upskilling orthoptists and ophthalmic trainees, and to improve their confidence before utilising this skill in a clinical setting
We advocate the use of this model to help improve the confidence of clinicians and the wellbeing of the patient.
The utility of Anti adalimumab antibodies (AAA) testing in paediatric uveitis patients - Thu 13.20 - 13.35
H.Razzouk (SAS), J.Ashworth (P), Manchester Royal Eye Hospital
Adalimumab is well established as a biologic immunosuppressive treatment for children with non-infectious uveitis. It is increasingly recognised that treatment failure can be caused by the development of anti-adalimumab antibodies. We aimed to determine how often we test for AAA, how often AAA are positive, and the clinical utility of the test
Retrospective study of patients in the peadiatric uveitis clinic who were on Adalimumab treatment for non-infectious uveitis. AAA was tested in the clinic when there was a concern about persistence or recurrent inflammation, or compliance issues
57 patients were on adalimumab as monotherapy (14%) ,Adalimumab with other DMARD treatment 85,8%
92.98% of patient had JIA/idiopathic uveitis
22.80% of patients were tested for AAA. 46% of those tested were positive for AAA
(10.52% for total number of patients)
The time between starting the treatment and the presence of AAA varied between 3 month to 12 years. Higher levels of AAA were associated with lower levels of serum Adalimumab. However, some cases had negative AAA with low level of Adalimumab. 50 % of AAA positive patients were on both methotrexate and Adalimumab, 33.3% were on Adalimumab as monotherapy, 16% were on mycophenolate with Adalimumab
The development of Anti-Adalimumab Antibodies may be a factor when treatment failure occurs in paediatric uveitis. It may develop from 3 months after treatment until many years (12 years in our study). Further study is needed to assess the risk factors of developing AAA and whether a combination with DMARD treatment would prevent from this process
Superior Oblique Tuck Surgery Outcomes: A 7-Year Data - Thu 15.40 - 15.55
Devina Gogi (C), Rebecca Lewis (O) Janice Hoole (O), Ian Simmons (C) – St James’s University Hospital, Leeds
To report the surgical outcomes of the superior oblique tuck procedure in the management of superior oblique palsies performed at a single centre over a 7-year period
This is a retrospective study of superior oblique tuck performed over a 7-year period between 2016-2023 at a single centre. We evaluated patient demographics, the angle of deviation pre- and post-surgery in prism dioptres (PD), complications (iatrogenic Brown’s Syndrome) and improvement of diplopia/ head tilt post-operatively.
18 eyes from 18 patients were identified. More than 60% of cases were congenital superior oblique palsy. 16/18 patients (96.91%) displayed a reduction in angle of deviation post-operatively and improvement of diplopia & head tilt. 4/18 patients (22.22%) experienced post-operative iatrogenic Brown’s syndrome but none of these required further corrective surgery. Overall, 4/18 patients (22.22%) required additional extraocular muscle surgery to reduce diplopia further.
Our centre started Superior oblique tuck surgery in 2016. This data shows promising initial results of this surgery with excellent surgical outcomes with regards to reduction of the angle of deviation, diplopia, head tilt and limited complications. It is now the preferred surgical option in our centre, in Superior oblique palsy with incomitant vertical deviations in downgaze.
Primary Isolated Amyloidosis Of Lateral Rectus: A Case Report - Fri 13.15 - 13.30
Devina Gogi (C), Janice Hoole (O), Ian Simmons (C), St James’s University Hospital, Leeds
We report a case of external ophthalmoplegia in a woman due to an uncommon form of amyloidosis exclusively affecting the lateral rectus muscle.
A 46-year-old woman was treated as orbital myositis of lateral rectus of the right eye with oral steroids & NSAIDS as her orbital magnetic resonance imaging showed fusiform enlargement of the right lateral rectus muscle, without tendon involvement. She had right lateral rectus resection to correct her distance esotropia and did well initially but presented 3 years later with significant limitation of abduction of the right eye which increased exponentially with time. Routine laboratory examinations were unremarkable. A systemic work-up showed no evidence of systemic amyloidosis. However, extraocular muscle/ conjunctival biopsy confirmed the diagnosis of amyloidosis.
Primary isolated amyloidosis in the extraocular muscle is exceedingly rare; only 13 such cases without systemic involvement have been reported in literature, over the last four decades. This condition should be included in the differential diagnosis of extraocular muscle enlargement and tissue biopsy should be performed for diagnostic purposes.
They say my child can't see - Fri 13.30 - 13.45
P Anketell (O), J Jackson (Op), S George (C), on behalf of the NOVIC team, Belfast Health & Social Care Trust, Belfast
Cerebral visual impairment (CVI) is the leading cause of visual impairment in children in the developing world (Rahi et al 2003). Visual behaviours in CVI are impacted on by individual’s current health and physical needs. In 2015, the neuro-ophthalmic vision impairment clinic (NOVIC) was developed in Belfast. NOVIC is a multidisciplinary clinic providing a collaborative investigation between ophthalmic and paediatric specialists shared through an outcome report.
Visual findings are recorded for all patients attending NOVIC. This study describes the visual outcomes of children with a diagnosis of CVI attending NOVIC between 2015 and 2019 inclusive. The database was interrogated to report ophthalmic findings, refractive error, presence of strabismus and visual field defects.
111 children (median age=4.71 years, range 0.29-17.09, female=46) attended the clinic. N=98 had a diagnosis of CVI. Visual ability ranged from 0.3logMAR to blindsight. The following findings were noted for those with CVI; 26.5% (n=26) had ocular anatomical changes, 76.5% of cases had a significant refractive error issued, 80.6% had strabismus, 63.3% had a visual field defect.
This study has provided an outline of the visual functions of patients with a diagnosis of CVI assessed in an MDT environment. The NOVIC MDT clinic facilitates collaboration between specialities and addresses common questions of ‘what can my child see?’ Outcomes from the clinic have influenced input for patients beyond health including education and housing. Further analyses of these subjective measures is underway which will provide a detailed picture of a large population of children with CVI.
Dominant Optic Atrophy: Diagnostic and Therapeutic Approach in the Paediatric Population - Fri 13.45 - 14.00
N Arruti (C), M Nieves-Moreno (C), P Rodriguez-Solana (RF), E Vallespin (C), S Noval (C), Hospital Universitario La Paz
To analyse the diagnostic and therapeutic approach in children diagnosed with Dominant Optic Atrophy (DOA).
Methods: Retrospective review of the paediatric patients’ medical records with confirmed DOA seen in the Paediatric Ophthalmology Department in the Hospital Universitario La Paz from the 1st of January 2018 to the 1st January 2022.
A total of 11 children were identified in the study period. The main initial complaint was reduced visual acuity, present in eight patients. Mean visual acuity at baseline was 0.37 in the right eye and 0.35 in the left eye (decimal scale). Mean visual acuity at the end of the study period was 0.38 and 0.35 right and left respectively. Optic Coherence Tomography at the first visit showed a mean retinal nerve fibre layer thickness of 81.6 microns in the right eye and 80.5 microns in the left eye and a mean ganglion cell layer of 52.5 and 52.4 microns right and left respectively. Most common visual field defect found was a centrocecal scotoma and nine out of eleven patients showed bilateral temporal disc pallor at baseline. Six patients are currently being treated with off-label idebenone maintaining visual acuity without any side effects.
After the OPA1 gene was sequenced, seven different OPA1 mutations were identified. Two of those, c.267G>A and c.1406_1407del have not been previously reported.
Our study adds two novel variants to the mutation spectrum of the OPA1 gene. Early diagnosis of DOA is crucial, both for avoiding unnecessary consultations and for an appropriate genetic counselling.
Max Rayne Foyer posters 17-18
ABSTRACTS
Click on the + sign to open up abstracts
Setting up a modern nurse led retinopathy of prematurity screening service at Imperial College Healthcare NHS Trust - Fri 13.30 - 13.45
C Hennings (T), P Patel (O), S Wren (C), Imperial College Healthcare NHS Trust
Nationally last year, 7295 babies were eligible for retinopathy of prematurity screening. Increasing premature births, limited resources in screening staff and intensive schedules require alternative approaches. Models for safe and effective neonatal nurse led screening have been touted for near a decade
Within a level 2 neonatal unit a standard operating procedure for babies to be screened by neonatal nurses using a wide field digital retinal imaging (WFDRI) camera was deployed. This required: cost analysis, procurement, competency-based training, secure data management and audit of national guidelines. Babies were concurrently screened with Binocular Indirect Ophthalmoscopy (BIO) to ensure safety.
The Panocam by Visunex Systems was selected. During a 6-month period, 25 babies were screened. All babies received initial and termination examination with BIO and were possible WFDRI. Overall WFDRI was used 43 times for screening. All babies were screened on time and within appropriate intervals. No baby missed reviews and there is no delay in referral for treatment.
Numerous challenges exist but with-it rewards. Choice of WFDRI is a balance between cost, usability and effectiveness. A safe SOP working within established protocols needs scrutiny. Data management ensuring balance of governance and usability is testing. Empowering our workforce to take on this challenge has allowed skill development that was otherwise unavailable.
We provide a base model for similar UK units to establish a ROP neonatal nurse lead digital screening program. We have shown it to be safe in its current deployment.
A rare case of bilateral optic nerve atrophy - Fri 13.45 - 14.00
M W Sarfraz (T), A Shafi (C), The Mid Yorkshire Hospitals NHS Trust, Wakefield
Optic atrophy is a leading cause of childhood visual impairment. It poses a diagnostic challenge and can be caused by ocular and systemic conditions. We present a case of Bosch-Boonstra-Schaaf Optic Atrophy Syndrome (BBSOAS), a rare neurological disorder characterized by a wide array of clinical features including optic atrophy, developmental delay and intellectual disability.
This 9-year-old girl was referred to us in 2021 for a second opinion regarding unexplained bilateral reduced vision (0.4 and 0.6). She had been first seen age 5months, with an intermittent exotropia and otherwise normal ocular exam. Aged 4years, she was re-referred by optician due to reduced vision (6/10 and 6/15) and found to have fine latent nystagmus and reduced vision bilaterally, with temporal optic disc pallor. Electrodiagnostics and neuroimaging were reported as normal. Other than monitoring for poor weight gain, she was systemically well. We performed optical coherence tomography (OCT) that showed a global reduction in the retinal nerve fibre and ganglion cell layers, suggesting bilateral optic atrophy. Genetic testing detected a pathogenic deletion of the NR2F1 gene, confirming a diagnosis of autosomal dominant BBSOAS.
This rare case highlights the importance of performing objective tests, like OCT and the usefulness of genetic testing in appropriate cases. As genetic testing has been “democratised”, it also leaves the ophthalmologist as the initial contact for parents with the results of genetic testing- therefore we must be equipped to signpost them to regional counselling services and specialist clinical centres, as well as guiding the family towards appropriate supportive resources.
Legend
(C) = Consultant, (O) = Orthoptist, (T) = Trainee, (CF) = Clinical Fellow, (CL) = Clinical Lecturer, (CRF) = Clinical Research Fellow, (F) = Fellow, (FD) = Foundation Doctor, (L) = Lecturer, (MS) = Medical Student, (N) = Nurse, (Op) = Optometrist, (P) = Professor, (RA) = Research Associate, (RF) = Research Fellow, (RO) = Research Orthoptist, (SAS) = Specialty Doctor, (SL) = Senior Lecturer, (o) = other

